Incontinence, often perceived as an inevitable part of ageing in the UK, can be an embarrassing and challenging condition for older people, particularly those with frailty and cognitive dysfunction.
Current guidelines on the management of urinary incontinence (UI) suggest that older adults who struggle with some degree of urinary incontinence often experience a decrease in their quality of life due to its prevalence as a common problem.
However, advancements in treatments and an increased understanding of the condition are making it possible for many older adults to manage, and in some cases, significantly reduce or even cure incontinence.
This article will explore the different types of incontinence, the causes behind it, and the available treatments. For detailed studies, see related literature that includes DOI references for further reading.
Benefits of Incontinence Direct EMS Chair Treatment for Incontinence in Older Adults
| Treatment | Invasiveness & Comfort | Suitability for Older Adults | Typical Convenience | Key Benefit Highlight | Considerations |
|---|---|---|---|---|---|
| Incontinence Direct EMS Chair (Emsella-style HIFEM) | Non-invasive; fully clothed, seated treatment; painless | Excellent for mobility-limited or frail adults; minimal physical effort needed | ~30-min sessions; no recovery time; integrates easily into routines | Stimulates thousands of pelvic floor contractions quickly; improves continence and quality of life with low burden | Access depends on clinic availability; may require multiple sessions; response varies |
| Pelvic Floor Physiotherapy (PFPT) & Biofeedback | Non-invasive; may involve physical exercises, probes, or guided training | Effective if cognitive & motor skills intact; may be challenging for some | Weekly sessions plus home exercises; compliance essential | Builds pelvic strength and awareness; long-term benefit | Requires commitment, memory, and possibly caregiver assistance |
| Dietary Changes / Medications | Non-invasive; oral or diet-based management | Easily managed if no swallowing or dietary restrictions | Daily habit-based, low time commitment | Helps regulate stool consistency and urgency | Doesn’t address muscle function; side-effects like constipation or medication interactions possible |
| Anal Bulking Injections | Minimally invasive; outpatient injections | Generally tolerated if minor procedural risk acceptable | Quick in-clinic procedure; occasional repeats needed | Enhances sphincter closure; reduces leakage episodes | Effects may diminish; some procedural discomfort; not for all FI causes |
| Nerve Stimulation (PTNS / SNS) | Minimally to moderately invasive; SNS requires implant, PTNS uses needle/electrodes | PTNS manageable; SNS surgical and may not suit frail individuals | PTNS: weekly clinic visits; SNS: surgery + follow-up | Modulates nerve reflexes; good efficacy in selected patients | Time-intensive (PTNS) or surgical risk (SNS); cost and maintenance considerations |
| Corrective Surgery (e.g., Sphincteroplasty) | Invasive surgical procedure | May be risky for older adults with frailty or comorbidities | One-time operation with post-surgical recovery | Directly repairs structural damage; can yield significant improvement | Surgical risks, anesthesia, recovery demands; benefits may decline long-term |
| Note: This comparison is illustrative. Older adults should consult healthcare professionals to choose the most appropriate treatment based on health status, mobility, and personal preferences. | |||||
Understanding Incontinence in Older Adults UK
Incontinence is the involuntary loss of bladder or bowel control, which can sometimes be associated with constipation. For older adults, this condition is often more prevalent due to ageing-related factors. It’s essential to recognise that incontinence is not a disease but rather a symptom that can result from various underlying health issues, particularly at the end of life. By addressing these factors, many older adults can see significant improvement in their condition.
There are several types of incontinence, each with its own causes and treatment options:
- Stress Incontinence: This occurs when physical activity, such as coughing, sneezing, or lifting heavy objects, puts pressure on the bladder, causing leakage. It is often due to weakened pelvic muscles.
- Urge Incontinence: Also known as overactive bladder (OAB), this is characterised by a sudden and intense urge to urinate, followed by involuntary loss of urine. Nerve damage, infections, or conditions like diabetes can cause it.
- Overflow Incontinence: This happens when the bladder doesn’t empty fully, leading to frequent dribbling. It is often related to bladder blockages or nerve issues.
- Functional Incontinence: This occurs when a person is unable to reach the bathroom in time due to physical or mental impairments. Cognitive issues like dementia or mobility challenges can lead to functional incontinence.
- Mixed Incontinence: A combination of two or more types of incontinence, commonly stress and urge incontinence.
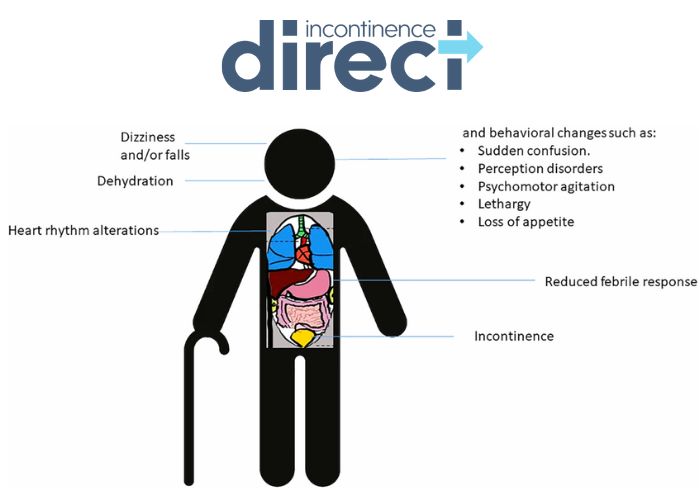
Causes of Incontinence in Older Adults UK
Ageing plays a significant role in increasing the risk of incontinence, but it is not the only factor. Incontinence in older adults can stem from various medical conditions, lifestyle factors, and medications.
- Pelvic Muscle Weakness: As people age, their pelvic floor muscles can weaken, especially in women who have experienced childbirth. Weak pelvic muscles make it harder to control bladder function.
- Chronic Health Conditions: Conditions like diabetes, Parkinson’s disease, and multiple sclerosis can damage the nerves that control bladder function. In men, an enlarged prostate can lead to overflow incontinence.
- Medications: Some medications, such as diuretics, can increase the frequency of urination, while others may relax bladder muscles, increasing the risk of leakage.
- Infections: Urinary tract infections (UTIs) can cause sudden and temporary incontinence by irritating the bladder.
- Cognitive Decline: Conditions like Alzheimer’s or dementia can prevent individuals from recognising the need to go to the bathroom or from physically being able to respond in time.
- Mobility Issues: Physical limitations, such as arthritis or injuries, may make it difficult for older adults to reach the bathroom in time, contributing to functional incontinence.
Treatment Options for Incontinence in Older Adults UK
The good news is that incontinence can often be managed, and in some cases, cured. The treatment depends on the type and severity of the incontinence, as well as the underlying causes.
1. Lifestyle Changes:
- Fluid Management: Limiting caffeine and alcohol, and managing fluid intake can help reduce the frequency of incontinence episodes.
- Dietary Adjustments: Certain foods, such as spicy foods or citrus fruits, can irritate the bladder and should be limited.
- Bladder Training: This technique involves scheduling bathroom trips and gradually increasing the time between urination to improve bladder control.
2. Pelvic Floor Exercises
Pelvic floor exercises, also known as Kegel exercises, can strengthen the muscles responsible for controlling urination. These exercises are efficient for stress incontinence and can significantly improve bladder control over time.
3. Medications
Depending on the type of incontinence, medications may be prescribed to relax bladder muscles, reduce urgency, or treat infections. Anticholinergics, beta-3 agonists, and estrogen therapy are some standard options.
4. Medical Devices
- Pessary: A small device inserted into the vagina (for women) to support the bladder and reduce leakage.
- Catheters: For individuals with overflow incontinence, using a catheter to drain the bladder can help prevent accidents.
- Electrical Stimulation: Devices that stimulate the pelvic muscles and nerves can help improve control over bladder function.
- Surgical Intervention: For more severe cases, surgery may be recommended. Procedures such as sling surgeries (to support the bladder) or Botox injections (to relax the bladder muscles) can provide long-term relief from incontinence.
5. Behavioural Therapy
Cognitive-behavioural therapy can help individuals with functional or urge incontinence understand and manage their condition better. This approach is beneficial for those with cognitive decline.
6. Absorbent Products
While these products don’t treat the condition, absorbent pads, adult diapers, and specialised underwear can help older adults manage incontinence and maintain dignity while seeking treatment.

Can Incontinence Be Cured?
The term “cured” can be complex when discussing the treatment of urinary incontinence in older adults, as it largely depends on the underlying cause, including factors like blood pressure.
However, with the right primary care treatment plan, many older adults can experience a significant reduction in symptoms, and in some cases, a complete resolution of incontinence. For instance, stress incontinence caused by weak pelvic muscles can be treated effectively with exercises and, if necessary, surgery.
For other types, such as urge incontinence, lifestyle changes and medications can significantly reduce the urgency and frequency of leakage episodes. While some older adults may not experience a complete cure, they can still manage their symptoms to the point where incontinence no longer impacts their daily lives.
Improving Quality of Life
Addressing incontinence can dramatically improve the quality of life for older adults. The emotional and psychological effects of incontinence, such as embarrassment, social withdrawal, and anxiety, can be as challenging as the physical symptoms. Fortunately, by taking steps toward treatment and management, older adults can regain control and confidence.
Incontinence should not be considered an inevitable part of ageing. With the right combination of lifestyle adjustments, medical treatments, and professional guidance, older adults can live with confidence and comfort.
How Our EMS (Electromagnetic Seat) Treatment UK Can Help You
We understand that managing incontinence can be a sensitive and frustrating experience, which is why we offer an advanced alternative to the Emsella treatment: the EMS (Electromagnetic Seat) Treatment. This non-invasive, comfortable therapy is designed to strengthen pelvic floor muscles and improve bladder control, helping individuals regain their confidence and quality of life.
What is EMS (Electromagnetic Seat) Treatment?
The EMS Treatment is an advanced form of pelvic floor therapy that uses focused electromagnetic energy to stimulate and strengthen the pelvic muscles. Similar to Emsella, this treatment helps restore muscle control in the pelvic region, but with enhanced technology to maximise results. The treatment is carried out while you sit on a special chair, which delivers high-intensity electromagnetic pulses directly to the pelvic floor area.
Each session lasts about 30 minutes and is non-invasive, meaning there is no need for surgery, anaesthesia, or recovery time. The treatment is suitable for both men and women suffering from various types of incontinence, including stress, urge, and mixed incontinence.
How Does EMS Work?
The EMS treatment works by triggering thousands of powerful muscle contractions in the pelvic floor area during each session. These contractions mimic the effect of intense pelvic exercises, such as Kegels, but at a much deeper level. As the muscles are stimulated, they regain strength and improve their ability to control the bladder.
For individuals with weakened pelvic muscles due to ageing, childbirth, or surgery, EMS treatment provides a highly effective solution to rebuild muscle tone and improve bladder control. This can lead to a noticeable reduction in incontinence symptoms after just a few sessions.

Benefits of EMS (Electromagnetic Seat) Treatment UK
- Non-Invasive and Painless: The EMS treatment is a completely non-invasive therapy, which means there is no need for surgery or needles. You sit on the EMS chair fully clothed while the treatment is administered, making it a stress-free experience with no downtime.
- Strengthens Pelvic Floor Muscles: One of the primary causes of incontinence is the weakening of the pelvic floor muscles. EMS treatment stimulates these muscles, promoting strength and endurance, which can significantly improve bladder control and reduce leakage.
- Quick and Convenient: Each session is only about 30 minutes long, allowing you to fit treatment into your schedule easily. Most patients start to see results after four to six sessions, making it a quick and effective way to address incontinence.
- Effective for Various Types of Incontinence: Whether you experience stress, urge, or mixed incontinence, EMS can target and improve symptoms across different types. By focusing on the pelvic floor, the treatment addresses the root cause of many incontinence issues.
- Safe and Comfortable: The treatment is entirely secure, with no reported side effects. Patients often describe the sensation as a series of gentle contractions, but there is no pain involved. You can sit back and relax during your session.
- Boosts Confidence and Quality of Life: Living with incontinence can impact your confidence and limit your social interactions. By improving bladder control, EMS treatment helps restore your ability to engage in daily activities without fear of leakage, giving you back your independence and self-assurance.
You can trust that you’re receiving top-quality care from our experienced professionals.
FAQs
Q: Can incontinence in older adults be cured?
A: While some forms of incontinence can be cured, particularly stress incontinence, others may be managed through lifestyle changes, pelvic exercises, medications, or surgical interventions, depending on the underlying causes.
Q: Are there non-surgical treatments for incontinence in older adults?
A: Yes, non-surgical treatments include pelvic floor exercises, medications, bladder training, and lifestyle adjustments such as dietary changes and fluid management.
Q: How can pelvic floor exercises help with incontinence in older adults?
A: Pelvic floor exercises, like Kegels, strengthen the muscles that support the bladder, which can improve bladder control, particularly for stress and urge incontinence.
Q: Is the treatment painful?
A: No, EMS treatment is painless. You may feel gentle muscle contractions during the session, but there is no discomfort.
Q: How long does each session last?
A: Each EMS session lasts approximately 30 minutes, making it a quick and convenient treatment option.
Q: Do I need to prepare for EMS treatment?
A: No special preparation is needed. You can wear your regular clothes and sit on the chair for the duration of the session.
Q: Is EMS treatment safe?
A: Yes, EMS treatment is safe and non-invasive, with no reported side effects.
Q: How long does it take to see results from EMS treatment?
A: Many patients begin to see improvement after four to six sessions, with full results typically achieved after eight sessions.

Take Control of Your Bladder Health
At Incontinence Direct, we believe in providing safe, effective, and non-invasive solutions for incontinence. Our EMS (Electromagnetic Seat) Treatment offers a modern, hassle-free way to strengthen your pelvic floor and take control of your bladder health. Whether you’re suffering from stress, urge, or mixed incontinence, EMS can help you regain your freedom and confidence without the need for surgery.
If you’re ready to explore how EMS treatment can improve your life, contact us today to schedule a consultation. Let us help you take the first step toward a life free from incontinence.
For Further Information, please call us on 03300100026